Women often explore various fertility options when trying to conceive later in life. One of the most frequently considered methods is insemination, which offers a less invasive path than many other fertility treatments. For those over 35, the outcomes can vary depending on several biological and medical factors.
As a woman ages, both the number and quality of eggs decline. This shift can influence the likelihood of a successful pregnancy through insemination. Still, many individuals achieve positive results through carefully planned care.
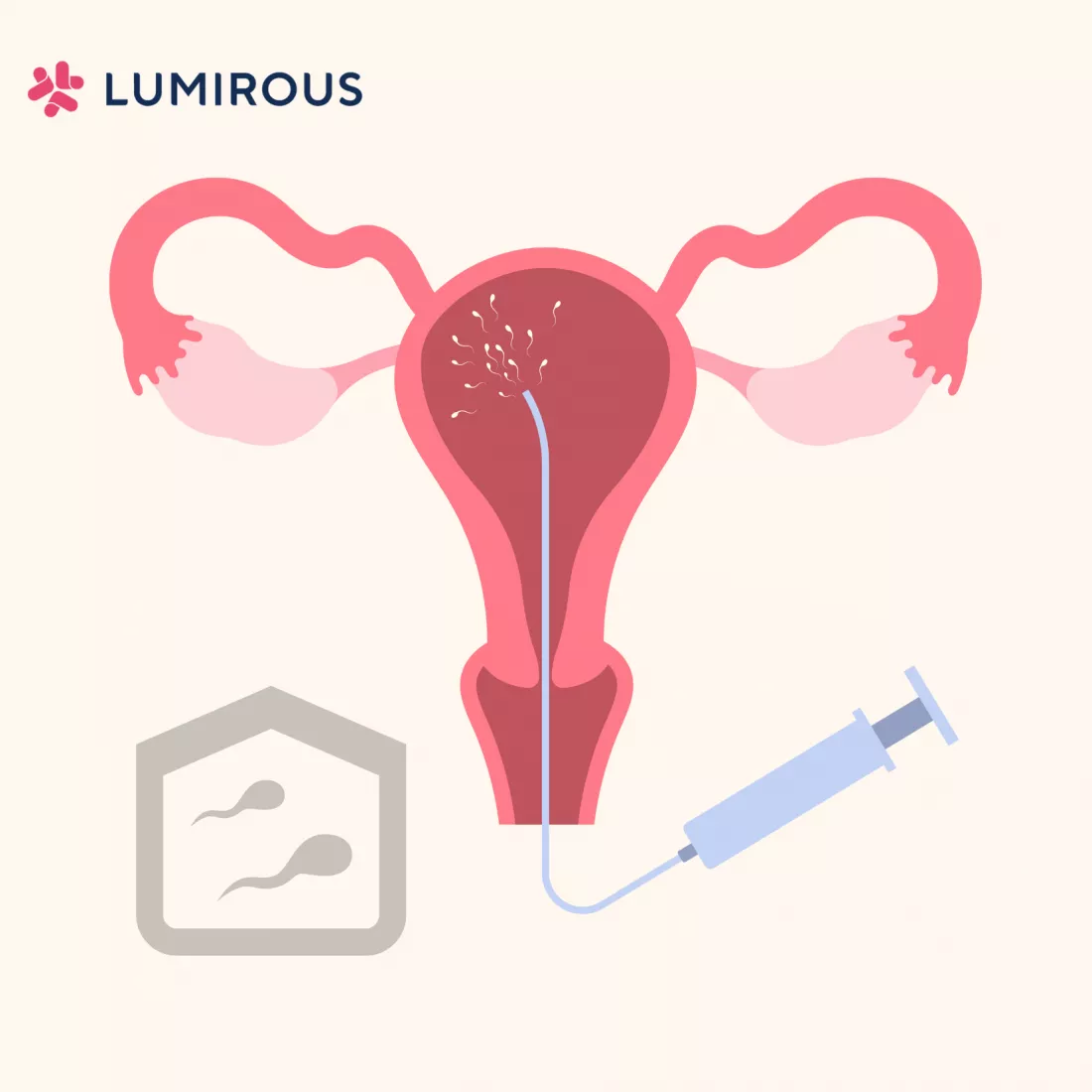
Understanding Insemination Methods
Insemination typically involves inserting prepared sperm directly into the uterus during ovulation. This process is known as intrauterine insemination, or IUI. The approach is often timed with fertility medication or ovulation tracking to improve the chance of success. Some individuals choose to use donor sperm, while others may work with a partner. In both cases, a fertility specialist provides guidance on timing, hormone levels, and overall reproductive health to support the process.
Tracking Success Rates by Age
For women under 35, the average success rate of IUI falls between fifteen to twenty percent per cycle. As age increases, those rates tend to decrease. Women aged 35 to 37 often see success rates closer to ten percent, while those in their early forties may experience even lower odds per cycle. Despite this, multiple cycles can increase the likelihood of conception over time. Some providers recommend up to three or four cycles before considering other treatment options.
A key factor in insemination success is ovarian reserve, or the number of viable eggs remaining. Providers may test hormone levels early in the treatment process to estimate how the body may respond. Tests such as AMH and FSH levels help determine whether hormone stimulation might be useful. These values also help guide decisions about timing, cycle planning, and whether insemination offers a realistic chance of success.
Supporting Treatments and Combined Strategies
Some fertility plans include the use of oral or injectable medications to stimulate ovulation. These treatments are often paired with insemination to increase the number of eggs released during a cycle. Ultrasounds and blood work are used to track progress and determine the ideal moment for insemination. When timed accurately, this approach can offer better odds than unmedicated cycles. Some individuals also explore lifestyle adjustments such as nutrition planning, stress management, or weight stabilization as part of a larger strategy.
If multiple cycles of insemination do not lead to pregnancy, many providers suggest a reevaluation. This does not always mean a change in treatment, but rather a deeper look at hormone function, uterine lining, and other physical factors. Advanced fertility treatments like in vitro fertilization may become part of the conversation at this stage. The decision to move forward with a new approach depends on goals, test results, and the advice of the care team.
Plan With a Fertility Specialist
Working with an experienced provider helps individuals understand their specific options. Each case includes different considerations based on age, medical history, and the results of fertility testing. Many fertility clinics offer tailored plans based on these details. Whether pursuing insemination alone or as part of a broader fertility journey, ongoing support and regular evaluations allow individuals to move forward with greater clarity.
- When to See a Foot and Ankle Surgeon
- Top Benefits of Visiting a Vein Clinic for Early Treatment of Vein Issues
- The Intersection of Gynecology and Endometriosis Treatment
- Regenerative Orthopedics for Post-Surgery Healing
- The Role of Pain Management in Living with Chronic Pain